- Home
- Our Doctors
- Our Offices
- New Patients
- Patient Education
- Blog
- Contact Us
- Patient Portal Help
- Product Center


Toenail fungus, or onychomycosis, is a common condition that can be both persistent and aesthetically bothersome. Traditional treatments like topical antifungal medications or oral prescriptions have limitations, prompting the exploration of innovative solutions such as laser therapy. Laser treatment for toenail fungus involves directing concentrated light energy onto the affected nails, effectively targeting the fungal infection without causing damage to the surrounding tissues. The high-intensity light penetrates the nail bed, disrupting the fungal cells and inhibiting their growth. While this method does not promise instantaneous results and may require multiple sessions, it offers a non-invasive alternative with minimal side effects compared to some conventional medications. Laser therapy is gaining popularity for its potential to enhance the appearance of affected nails and address the root cause of the fungal infection. Consulting with a podiatrist can provide valuable insights into whether laser treatment is a suitable option for addressing toenail fungus and restoring healthier, clearer nails. If you have toenail fungus, it is suggested that you confer with this type of doctor who can determine if this is a correct treatment option for you.
Laser treatment can be an effective way to get rid of toenail fungus. If you have any questions about laser treatment, consult with one of our podiatrists from Foot & Ankle Institue. Our doctors will assess your condition and provide you with quality treatment for fungal nails.
What Are Toenail Fungal Infections?
Onychomycosis, or fungal infection of the nail, is a relatively common and non-serious condition. Around 10 percent of U.S. citizens are afflicted with fungal nails. Common forms of fungus that infect the nail include dermatophytes, yeasts, and molds.
Symptoms of Toenail Fungal Infections Include:
Diagnosis for Fungal Nails
Fungal infections are diagnosed by fungal culture and microscopy. This will rule out any other conditions such as nail trauma, psoriasis, lichen planus, and onychogryphosis.
What Is Laser Treatment?
Laser treatment is a non-invasive, safe, quick, and painless procedure that uses the heat from a laser to kill fungus in the nail. Each infected nail is targeted with a laser for several minutes. The treatment is usually utilized several different times over a select period. During this time, a podiatrist will keep an eye on the infection.
If you have any questions, please feel free to contact one of our offices located in St. George, Hurricane, and Cedar City, UT and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A new treatment for fungal nails, or onychomycosis, which has grown in popularity in recent years, is laser treatment. Laser treatment involves the use of a laser that kills fungus in the toenail with heat. Laser therapy causes no side effects and does not affect nearby healthy tissue.
Toenail fungus afflicts almost 10 percent of the U.S. population and is more common among the elderly. The most common symptom of toenail fungus is the discoloration and thickening of the nail. The nail can also become brittle and a foul smell may be produced. In rare cases, pain might be present. While it is not a serious condition, it can lead to a perception of disgust amongst those it affects. There are several different fungi that cause fungal infections. These include dermatophyte, yeast, and mold. The most common of these is dermatophyte.
Diagnosis for fungal nails involves a podiatrist utilizing microscopy and fungal cultures. This will allow the doctor to determine whether it is a fungus or another condition, such as lichen planus, psoriasis, nail damage, and onychogryphosis.
Fungus in the nails can be hard to get rid of with over-the-counter drugs. This is due to the nail being hard and protective, with fungus able to slip between the nail bed and plate. Furthermore the slow growth of the nail increases the difficulty of fungus going away. Laser treatment seeks to get around this by directly penetrating through the nail and killing the fungus. The laser is used on each infected nail for a couple of minutes. Patients then typically return several weeks or months later for another laser treatment. During this time the podiatrist will routinely observe the foot and infection. It is also recommended to wear clean socks and shoes and allow the feet to dry and breathe to prevent toenail fungus.
Laser treatment is still a relatively new treatment and not all podiatrists have laser machines. Ask your podiatrist if they do laser treatment for toenail fungus and if it is right for you.

A foot stress fracture, a microscopic crack in a bone, can bring discomfort and disruption to one's daily activities. Typically caused by repetitive stress and overuse, these fractures often occur in weight-bearing bones, such as the metatarsals. These bones often endure more force than they can handle, leading to tiny cracks that, when compounded over time, manifest as stress fractures. Athletes engaging in high-impact activities, dancers, and military personnel are particularly susceptible due to the repetitive nature of their routines. Factors like sudden increases in activity intensity, improper footwear, or inadequate recovery periods can elevate the risk. Early recognition of symptoms such as localized pain, swelling, and tenderness is essential for timely intervention. Adopting preventive measures, such as a gradual increase in activity levels, and incorporating rest into routines can significantly decrease the risk of foot stress fractures. If you have developed a foot stress fracture, it is suggested that you confer with a podiatrist who can offer the treatment method that is right for you.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact one of our podiatrists from Foot & Ankle Institue. Our doctors can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact one of our offices located in St. George, Hurricane, and Cedar City, UT and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
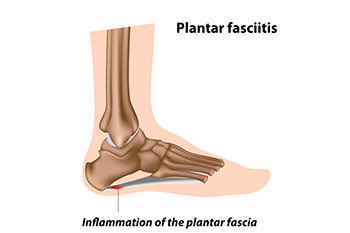
Plantar fasciitis, a common foot ailment affecting people between 25 and 65 years old, results from the overloading or overstretching of the plantar fascia, which is the supportive tissue beneath the foot's arch. A podiatrist may offer a variety of treatment options tailored to manage the pain of plantar fasciitis and help toward healing. Rest and support are integral to short-term management. Utilizing a walking boot and crutches allows the foot to rest, aiding in the recovery process. Corticosteroid injections become a consideration in cases of severe pain and inflammation resistant to other conservative treatments. However, caution is warranted due to potential weakening of the plantar fascia and the risk of rupture, which can lead to chronic pain and foot flattening. Extracorporeal shockwave therapy is a noninvasive procedure used by some podiatrists to stimulate healing in plantar fascia tissue. However, its effectiveness varies among individuals. Low-level laser therapy is sometimes employed by podiatrists to reduce the pain and inflammation associated with plantar fasciitis, offering relief for up to three months. In cases where nonsurgical treatments prove insufficient, foot surgery may be considered. But it typically is reserved for situations where significant improvement has not been observed through other methods. To find out more healing from plantar fasciitis, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment plan.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Foot & Ankle Institue. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in St. George, Hurricane, and Cedar City, UT and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.

One of the most important components of your foot is the big toe joint, scientifically known as the first metatarsophalangeal joint, or first MPJ. When issues arise within this joint, they can significantly impact your daily life, ranging from walking to overall body posture. Hallux limitus is a condition that pertains to the limited range of motion in the big toe joint. One of the main causes of this condition is inflammatory arthritis. Your big toe joint plays a critical role in walking and maintaining proper balance. When this joint loses its range of motion it can lead to significant difficulties in walking and cause pain during each step. This can alter the gait and in turn affect the knee, hip, and back. If arthritis is a contributing factor, disease specific medications can be prescribed. In severe cases, surgical intervention may be needed. Procedures can range from cleaning out the joint to more advanced surgeries, such as joint fusion or joint replacement. For an accurate appraisal of the problems involving your big toe pain, it is suggested that you make an appointment with a podiatrist.
Toe pain can disrupt your daily activities. If you have any concerns, contact one of our podiatrists of Foot & Ankle Institue. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
When to See a Podiatrist
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact one of our offices located in St. George, Hurricane, and Cedar City, UT and Mesquite, NV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.

There are two sesamoid bones located beneath the big toe which aid its movement. Problems with these sesamoid bones can vary from acute injuries such as turf toe, where the toe excessively bends due to fractures. Pain may also arise from sesamoiditis, an inflammation of the sesamoids, or from arthritis affecting the toe. Symptoms of acute sesamoid issues can manifest as intense pain and difficulty in walking, while chronic conditions may cause persistent pain under the big toe, which can be aggravated by certain shoes or activities, hinting at sesamoiditis. Diagnosis typically involves examining the patient's medical history and symptoms, supported by X-rays or more detailed scans such as an MRI or CT scan. Treatment strategies for sesamoid problems range from wearing supportive footwear and activity modifications. If these measures fail, surgery might be considered, which could include removing the sesamoid bones or repairing them. If you have foot pain of any sort, it is strongly suggested that you make an appointment with a podiatrist who can accurately diagnose the problem and offer treatment options that can help you return to normal activity levels.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of our podiatrists of Foot & Ankle Institue. Our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact one of our offices located in St. George, Hurricane, and Cedar City, UT and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Having issues or need help with your portal?
Click here for Instructional Videos